The WHO establishes a Human Reproduction Unit with the mandate to advise Member States about family planning. WHA “REQUESTS the Director-General to develop further the programmes proposed … in the fields of reference services, studies on medical aspects of sterility and fertility control methods and health aspects of population dynamics”
(WHA Resolution 18.49; 1965).
World Health Assembly passes Resolution WHA20.41 “to continue to develop the activities of the World Health Organization in the field of health aspects of human reproduction” considering that abortion and high maternal and child mortality rates constitute a serious health problem in many countries.

A feasibility study
(supported by the Government of Sweden) demonstrates the need for the UN system to expand research in human reproduction, emphasizing fertility regulation.
WHO establishes the Expanded Programme of Research, Development and Research Training in Human Reproduction “with the aim of developing a variety of safe, acceptable and effective methods of fertility regulation and of monitoring the long-term safety and efficacy of existing methods as well as the support of institutions capable of conducting such work”. The birth of HRP!
The definition of “acceptability” of fertility regulating methods is coined which is still universally accepted.
WHO first articulates the concept of sexual health: “the integration of the somatic, emotional, intellectual and social aspects of sexual being, in ways that are positively enriching and that enhance personality, communication and love.”
HRP conducts a collaborative study on the effectiveness of cervical mucus/ovulation method for natural family planning. It’s hailed as the first objective and unbiased evaluation of this method.
HRP organizes the first WHO Scientific Group on Induced Abortion.
A ten-year, 13-centre HRP study, the largest of its kind, provides firm evidence of safety of oral contraceptives with regard to the risk of cancer.

HRP publishes the first WHO laboratory manual for the examination and processing of human semen. In its sixth edition, this continues to be one of the WHO’s most downloaded publications.
HRP supports a study that shows nurse-midwives with proper training can insert and remove IUDs as safely as physicians.

Clinical trial results demonstrate that the administration of a prostaglandin analogue after mifepristone pre-treatment significantly improves abortion interventions. This is crucial for the development of medical abortion regimens.
HRP becomes an interagency programme, co-sponsored by UNDP, UNFPA, WHO and the World Bank, with WHO acting as executing agency. The HRP Policy and Coordination Committee is established as its formal governing body: “To coordinate, promote, conduct and evaluate international research in human reproduction”.
(WHA Resolution 41.9; 1988)
HRP undertakes large clinical studies on long-acting injectable contraceptives which contributes to their present worldwide availability and to the development and marketing of two combined oestrogen-progestin formulations that are injected once a month.
HRP conducts the largest ever study of the duration of lactational amenorrhea in relation to breast-feeding practices, proving this is a viable option for postpartum contraception. This study also showed that both breast-feeding behaviour and the duration of lactational amenorrhea vary across settings, and breast-feeding stimulus is strongly linked to the duration of postpartum amenorrhea.


WHO publishes the first synthesis of available data on abortion in 1990. This leads to the first estimates and to the adoption of a definition for unsafe abortion in 1993.
HRP conducts several randomised controlled trials exploring the safety and efficacy of misoprostol and mifepristone in combination and misoprostol alone for the medical management of abortion, working with 15 medical centres and three academic institutions.
WHO’s “Collaborative Study of Neoplasia and Steroid Contraceptives” provides information about the safety of oral and injectable contraceptives, and about other factors affecting cancer risk such as parity, lactation, and sexual behaviour.

HRP reviews data of 23 000 IUD users (from 12 studies) and finds that the risk of pelvic inflammatory disease is minimal in women at low risk of sexually transmitted infections and that the risk does not increase with long-term IUD use.
WHO Technical Working Group on the Prevention and Management of Unsafe Abortion is established to discuss WHO’s support to countries in norm-setting and standards. This meeting coins the definition of unsafe abortion which is internationally accepted and commonly used.
First registration of Mesigyna and Cyclofem, a once-a-month combined injectable contraceptive developed by HRP.
On the basis of data generated from HRP-supported research, the US Food and Drug Administration approves the extension of the lifespan of the copper IUD (CuT380A) to ten years.

The landmark International Conference on Population and Development (ICPD) in Cairo adopts a comprehensive definition of reproductive health that is developed with help from HRP. This paradigm shift in population policies is adopted by 179 countries.
At ICPD diverse views on human rights, population, sexual and reproductive health, gender equality and sustainable development merged into a global consensus that placed individual dignity and human rights, including the right to plan one’s family, at the heart of development.
“All countries should strive to make accessible through the primary health-care systems, reproductive health to all individuals of appropriate ages as soon as possible and no later than the year 2015.”
(ICPD Programme of Action, para. 7.6)

HRP completes a major study that shows that oral contraceptives can be safely used by young women who are non-smokers. This study also shows an increased risk of blood clots for certain types of oral contraceptives.

WHO publishes the first “Medical Eligibility Criteria for Contraceptive Use” which presents the latest WHO guidance on the safety of different contraceptive methods for women with specific health conditions and characteristics. It is now in its fifth edition.
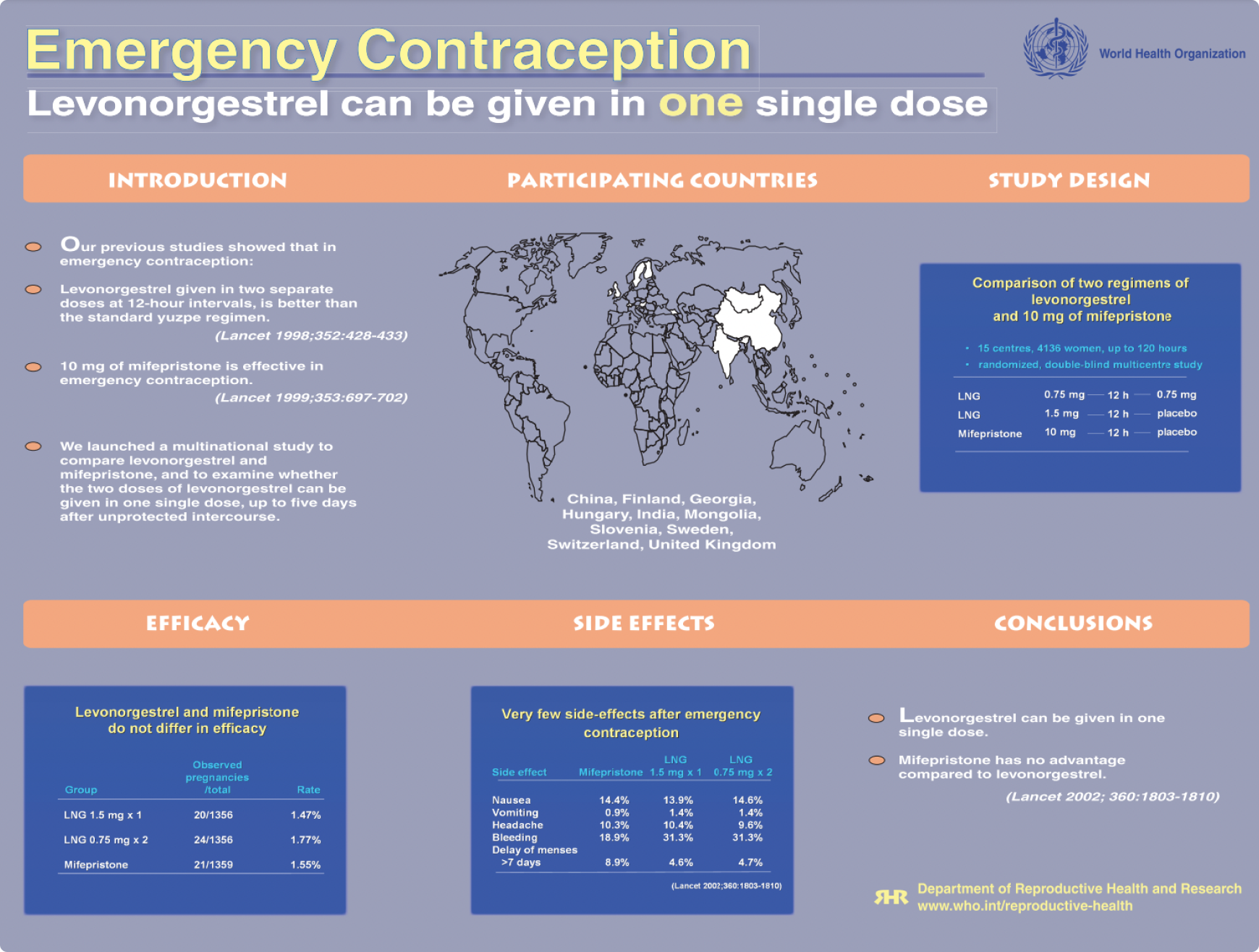
HRP plays a pioneering role in emergency contraception by confirming the effectiveness of levonorgestrel for emergency contraception, which results in changes in regulations in both developed and developing countries and its inclusion in the list of essential medicines by WHO. Since 1998 these pills have been licensed in more than 100 countries.

“Abortion in the Developing World”, a book summarizing results from 23 studies on the determinants of induced abortion is published. This book provides the most complete scientific information on the determinants of induced abortion in developing countries of Africa, Asia, and Latin America.
HRP convenes a group of 60 international experts to revisit the WHO definition of sexual health.
HRP research shows magnesium sulfate (a cheap, commonly available drug) can halve the risks and possible death of high blood pressure in pregnant women.

HRP’s research into emergency contraception shows that a single dose of levonorgestrel taken orally is safe and effective.
HRP evidence results in the first-ever guideline on abortion: “Safe Abortion: Technical and Policy Guideline for Health Systems”.
HRP makes a major contribution to the development and adoption of the World Health Assembly’s Global Reproductive Health Strategy.

HRP randomised controlled trials exploring the safety and efficacy of misoprostol and mifepristone contributes to the decision to add the combination of mifepristone followed by misoprostol to the WHO complementary List of Essential Medicines as a medical abortion regimen and important reproductive health medication.

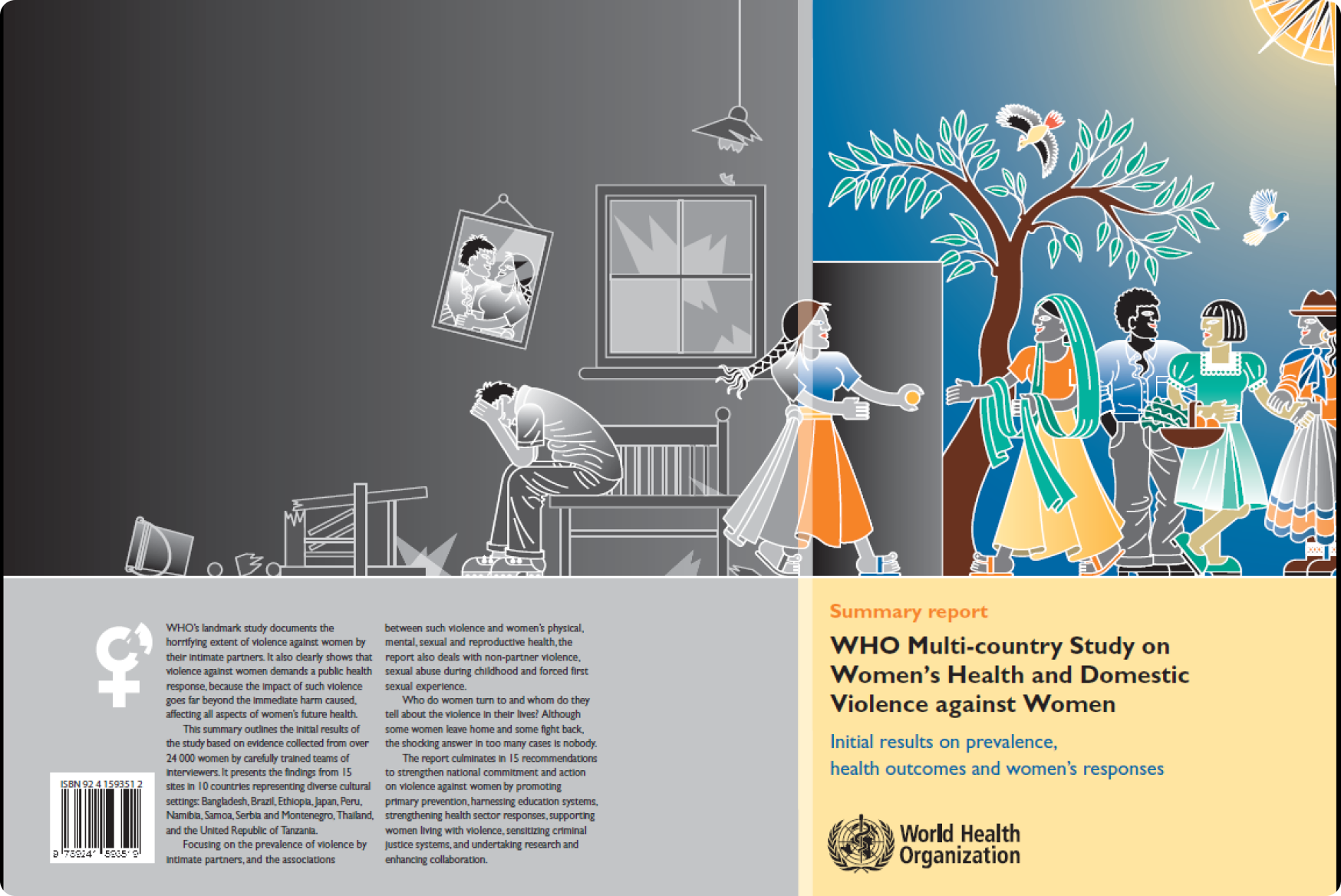
HRP publishes the first international prevalence data on women’s health and domestic violence revealing widespread violence by male partners in ten countries studied.
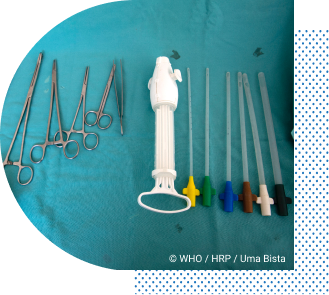
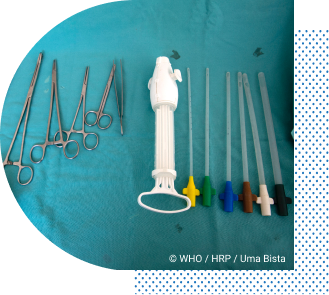
In the first-ever comparative randomized trial, HRP research provides the evidence that mid-level health care providers can perform first-trimester induced abortion using manual vacuum aspiration (MVA) as safely as physicians.
HRP leads a prospective study examining the effects of different types of Female Genital Mutilation on obstetric outcomes in over 28,000 women in Burkina Faso, Ghana, Kenya, Nigeria, Senegal, and Sudan. It found that FGM was associated with significantly greater risk of complications during childbirth and higher death rates among infants.
HRP’s working group looking at the definition of sexual health recommends and publishes working definitions of ‘sexual health’, ‘sex’, ‘sexuality’ and ‘sexual rights’, thus reasserting sexual health as a key aspect of the human experience throughout the life-course. This remains in use today by the WHO.
HRP’s report on the persistence of unsafe abortion and its public health consequences receives wide international coverage in media and international debate on reproductive health.
The first edition of the WHO’s joint publication “Family Planning: A Global Handbook for Providers” is released. Now in its fourth edition, it is the most widely used reference guide on the topic globally, with over a million copies distributed or downloaded to date. Support for its production and dissemination has been provided through the Johns Hopkins Bloomberg School of Public Health and the United States Agency for International Development (USAID).
Data from an HRP multinational study on medical abortion are used by the Concept Foundation to prepare a registration file of a two-drug product (mifepristone and misoprostol). Negotiations with the manufacturer result in the establishment of a substantially lower price for the public sector in developing countries.
HRP’s work on the Kesho Bora Study (“Preventing mother-to-child transmission of HIV during breastfeeding”) shows a combination of antiretroviral drugs during pregnancy and delivery was safe and efficacious. The findings strongly influence the revision of the WHO guidelines on antiretrovirals, prevention of mother-to-child transmission of HIV and infant feeding issued in July 2010.

WHO publishes the “Global strategy to stop health care providers from performing female genital mutilation” in collaboration with other key UN agencies and international organizations.
HRP study on the “Active management of the third stage of labour with and without controlled cord traction” concludes that omission of controlled cord traction has very little effect on the risk of severe haemorrhage in settings where skilled birth attendants are not available.
The second edition of the “Safe Abortion: Technical and Policy Guidance for Health Systems” is published.
The WHO publishes the global and regional estimates of violence against women as well as clinical and policy recommendations on responding to intimate partner violence and sexual violence against women.
UNICEF and UNAIDS join HRP’s governing body.
HRP research results in a WHO statement on the prevention and elimination of disrespect and abuse during facility-based childbirth, one of the most translated WHO documents.
In response to the global emergency of the Ebola epidemic in West Africa, HRP teamed with WHE, WHO and the government of Sierra Leone to, together with China and US CDC develop an emergency research response to analyze presence of Ebola virus in semen and other body fluids. The study was coordinated by HRP and provided groundbreaking results related to presence over time of Ebola viral RNA in semen. Emerging study results were applied to WHO Emergency Guidance on reduction of sexual transmission of Ebola, developed by HRP and WHE colleagues.
HRP leads the development of a new comprehensive guideline on routine antenatal care for pregnant women. This leads to the “2016 WHO recommendations on antenatal care for a positive pregnancy experience” and on a thorough review of the evidence, introduced the 2016 WHO ANC model to replace the 2002 FANC model. The 2016 ANC recommendations are one of three evidence-based guidelines that HRP developed to improve quality of care for women and their babies throughout the pregnancy, childbirth, and postnatal continuum.

HRP through a seven-year FU clinical trial in seven countries documented the effectiveness, efficacy and side effects of single, and two rods subdermal implants, and IUD. It publishes an article “Extended use up to 5 years of the etonogestrel-releasing subdermal contraceptive implant: comparison to levonorgestrel-releasing subdermal implant.”
With HRP input, the WHO in collaboration with the UNFPA-UNICEF Joint Programme on FGM launched the first evidence-based guidelines on the management of health complications from FGM.
HRP research contributes to the WHO recommendations on intrapartum care for a positive childbirth experience.
HRP uses the findings from the Global Early Adolescent Study to advocate for equitable gender norms in the 2018 update of the UN “International Technical Guidance on Comprehensive Sexuality Education”.
Medical Eligibility Criteria Wheel for Contraceptive Use (or MEC wheel) is made available digitally via an app.
HRP publishes the first multi-country effort on the mistreatment of women during childbirth.
HRP publishes that demand-side financing such as vouchers in family planning are effective in increasing use, improving equity and reaching the underserved in enhancing and contributing to UHC.
Together with the WHO, HRP publishes the first consolidated guideline on self-care interventions for health presenting existing and new recommendations to support access to, uptake of, and use of self-care interventions, particularly for sexual and reproductive health and rights, based on the best available evidence.
HRP conducts research to identify inequities in Latin America and the Caribbean with a focus on long-acting reversible contraceptives in 23 countries.
HRP demonstrates that the efficacy and safety of heat-stable carbetocin is comparable with oxytocin (the gold standard intervention) for the prevention of postpartum haemorrhage.
HRP launches the Female Genital Mutilation Cost Calculator, an interactive tool demonstrating the projected costs of treatment of health complications under different scenarios of FGM prevention.
The WHO launches the SRHR Policy Portal as an interactive tool to visualize global health data on Sexual and Reproductive Health including country and region specific SRHR indicators.
The first-ever comprehensive definition of family planning counselling is published. HRP develops this in collaboration with others.
HRP Statistics Portal is launched to HRP researchers and collaborators as an innovative tool aimed at strengthening capacity in statistics and data management in research. It serves as a useful resource for accessing technical material and information regarding statistics, data management and international standard guidelines for ethics, conducting, monitoring and reporting of SRH research.
HRP launches ethical guidance on conducting research on FGM complementing the launch of the research agenda on FGM by UNICEF, WHO, HRP, UNFPA and Population Council.
The third comprehensive update of the “Abortion Care Guideline” is published. It consolidates over 50 recommendations on the clinical, service delivery, legal and human rights aspects of providing abortion care.
HRP publishes the report “Infertility Prevalence Estimates: 1990-2021”, the first report of its kind in over a decade.

The WHO establishes a Human Reproduction Unit with the mandate to advise Member States about family planning. WHA “REQUESTS the Director-General to develop further the programmes proposed … in the fields of reference services, studies on medical aspects of sterility and fertility control methods and health aspects of population dynamics”
(WHA Resolution 18.49; 1965).
World Health Assembly passes Resolution WHA20.41 “to continue to develop the activities of the World Health Organization in the field of health aspects of human reproduction” considering that abortion and high maternal and child mortality rates constitute a serious health problem in many countries.

A feasibility study
(supported by the Government of Sweden) demonstrates the need for the UN system to expand research in human reproduction, emphasizing fertility regulation.
WHO establishes the Expanded Programme of Research, Development and Research Training in Human Reproduction “with the aim of developing a variety of safe, acceptable and effective methods of fertility regulation and of monitoring the long-term safety and efficacy of existing methods as well as the support of institutions capable of conducting such work”. The birth of HRP!
The definition of “acceptability” of fertility regulating methods is coined which is still universally accepted.
WHO first articulates the concept of sexual health: “the integration of the somatic, emotional, intellectual and social aspects of sexual being, in ways that are positively enriching and that enhance personality, communication and love.”
HRP organizes the first WHO Scientific Group on Induced Abortion.
A ten-year, 13-centre HRP study, the largest of its kind, provides firm evidence of safety of oral contraceptives with regard to the risk of cancer.

HRP publishes the first WHO laboratory manual for the examination and processing of human semen. In its sixth edition, this continues to be one of the WHO’s most downloaded publications.

HRP supports a study that shows nurse-midwives with proper training can insert and remove IUDs as safely as physicians.

Clinical trial results demonstrate that the administration of a prostaglandin analogue after mifepristone pre-treatment significantly improves abortion interventions. This is crucial for the development of medical abortion regimens.
HRP becomes an interagency programme, co-sponsored by UNDP, UNFPA, WHO and the World Bank, with WHO acting as executing agency. The HRP Policy and Coordination Committee is established as its formal governing body: “To coordinate, promote, conduct and evaluate international research in human reproduction”.
(WHA Resolution 41.9; 1988)
HRP undertakes large clinical studies on long-acting injectable contraceptives which contributes to their present worldwide availability and to the development and marketing of two combined oestrogen-progestin formulations that are injected once a month.
HRP conducts the largest ever study of the duration of lactational amenorrhea in relation to breast-feeding practices, proving this is a viable option for postpartum contraception. This study also showed that both breast-feeding behaviour and the duration of lactational amenorrhea vary across settings, and breast-feeding stimulus is strongly linked to the duration of postpartum amenorrhea.


WHO publishes the first synthesis of available data on abortion in 1990. This leads to the first estimates and to the adoption of a definition for unsafe abortion in 1993.
HRP conducts several randomised controlled trials exploring the safety and efficacy of misoprostol and mifepristone in combination and misoprostol alone for the medical management of abortion, working with 15 medical centres and three academic institutions.
WHO’s “Collaborative Study of Neoplasia and Steroid Contraceptives” provides information about the safety of oral and injectable contraceptives, and about other factors affecting cancer risk such as parity, lactation, and sexual behaviour.

HRP reviews data of 23 000 IUD users (from 12 studies) and finds that the risk of pelvic inflammatory disease is minimal in women at low risk of sexually transmitted infections and that the risk does not increase with long-term IUD use.
WHO Technical Working Group on the Prevention and Management of Unsafe Abortion is established to discuss WHO’s support to countries in norm-setting and standards. This meeting coins the definition of unsafe abortion which is internationally accepted and commonly used.
First registration of Mesigyna and Cyclofem, a once-a-month combined injectable contraceptive developed by HRP.

On the basis of data generated from HRP-supported research, the US Food and Drug Administration approves the extension of the lifespan of the copper IUD (CuT380A) to ten years.



HRP completes a major study that shows that oral contraceptives can be safely used by young women who are non-smokers. This study also shows an increased risk of blood clots for certain types of oral contraceptives.

WHO publishes the first “Medical Eligibility Criteria for Contraceptive Use” which presents the latest WHO guidance on the safety of different contraceptive methods for women with specific health conditions and characteristics. It is now in its fifth edition.
HRP plays a pioneering role in emergency contraception by confirming the effectiveness of levonorgestrel for emergency contraception, which results in changes in regulations in both developed and developing countries and its inclusion in the list of essential medicines by WHO. Since 1998 these pills have been licensed in more than 100 countries.

“Abortion in the Developing World”, a book summarizing results from 23 studies on the determinants of induced abortion is published. This book provides the most complete scientific information on the determinants of induced abortion in developing countries of Africa, Asia, and Latin America.
HRP convenes a group of 60 international experts to revisit the WHO definition of sexual health.
HRP research shows magnesium sulfate (a cheap, commonly available drug) can halve the risks and possible death of high blood pressure in pregnant women.
HRP’s research into emergency contraception shows that a single dose of levonorgestrel taken orally is safe and effective.
HRP evidence results in the first-ever guideline on abortion: “Safe Abortion: Technical and Policy Guideline for Health Systems”.
HRP makes a major contribution to the development and adoption of the World Health Assembly’s Global Reproductive Health Strategy.

HRP randomised controlled trials exploring the safety and efficacy of misoprostol and mifepristone contributes to the decision to add the combination of mifepristone followed by misoprostol to the WHO complementary List of Essential Medicines as a medical abortion regimen and important reproductive health medication.

HRP publishes the first international prevalence data on women’s health and domestic violence revealing widespread violence by male partners in ten countries studied.
In the first-ever comparative randomized trial, HRP research provides the evidence that mid-level health care providers can perform first-trimester induced abortion using manual vacuum aspiration (MVA) as safely as physicians.
HRP leads a prospective study examining the effects of different types of Female Genital Mutilation on obstetric outcomes in over 28,000 women in Burkina Faso, Ghana, Kenya, Nigeria, Senegal, and Sudan. It found that FGM was associated with significantly greater risk of complications during childbirth and higher death rates among infants.
HRP’s working group looking at the definition of sexual health recommends and publishes working definitions of ‘sexual health’, ‘sex’, ‘sexuality’ and ‘sexual rights’, thus reasserting sexual health as a key aspect of the human experience throughout the life-course. This remains in use today by the WHO.
HRP’s report on the persistence of unsafe abortion and its public health consequences receives wide international coverage in media and international debate on reproductive health.
The first edition of the WHO’s joint publication “Family Planning: A Global Handbook for Providers” is released. Now in its fourth edition, it is the most widely used reference guide on the topic globally, with over a million copies distributed or downloaded to date. Support for its production and dissemination has been provided through the Johns Hopkins Bloomberg School of Public Health and the United States Agency for International Development (USAID).
Data from an HRP multinational study on medical abortion are used by the Concept Foundation to prepare a registration file of a two-drug product (mifepristone and misoprostol). Negotiations with the manufacturer result in the establishment of a substantially lower price for the public sector in developing countries.
HRP’s work on the Kesho Bora Study (“Preventing mother-to-child transmission of HIV during breastfeeding”) shows a combination of antiretroviral drugs during pregnancy and delivery was safe and efficacious. The findings strongly influence the revision of the WHO guidelines on antiretrovirals, prevention of mother-to-child transmission of HIV and infant feeding issued in July 2010.

WHO publishes the “Global strategy to stop health care providers from performing female genital mutilation” in collaboration with other key UN agencies and international organizations.
HRP study on the “Active management of the third stage of labour with and without controlled cord traction” concludes that omission of controlled cord traction has very little effect on the risk of severe haemorrhage in settings where skilled birth attendants are not available.
The second edition of the “Safe Abortion: Technical and Policy Guidance for Health Systems” is published.
UNICEF and UNAIDS join HRP’s governing body.
HRP research results in a WHO statement on the prevention and elimination of disrespect and abuse during facility-based childbirth, one of the most translated WHO documents.

With HRP input, the WHO in collaboration with the UNFPA-UNICEF Joint Programme on FGM launched the first evidence-based guidelines on the management of health complications from FGM.
HRP research contributes to the WHO recommendations on intrapartum care for a positive childbirth experience
HRP uses the findings from the Global Early Adolescent Study to advocate for equitable gender norms in the 2018 update of the UN “International Technical Guidance on Comprehensive Sexuality Education”.
HRP publishes the first multi-country effort on the mistreatment of women during childbirth.
HRP publishes that demand-side financing such as vouchers in family planning are effective in increasing use, improving equity and reaching the underserved in enhancing and contributing to UHC.
HRP conducts research to identify inequities in Latin America and the Caribbean with a focus on long-acting reversible contraceptives in 23 countries.
HRP demonstrates that the efficacy and safety of heat-stable carbetocin is comparable with oxytocin (the gold standard intervention) for the prevention of postpartum haemorrhage.
HRP demonstrates that the efficacy and safety of heat-stable carbetocin is comparable with oxytocin (the gold standard intervention) for the prevention of postpartum haemorrhage.
HRP launches the Female Genital Mutilation Cost Calculator, an interactive tool demonstrating the projected costs of treatment of health complications under different scenarios of FGM prevention
The WHO launches the SRHR Policy Portal as an interactive tool to visualize global health data on Sexual and Reproductive Health including country and region specific SRHR indicators


HRP Statistics Portal is launched to HRP researchers and collaborators as an innovative tool aimed at strengthening capacity in statistics and data management in research. It serves as a useful resource for accessing technical material and information regarding statistics, data management and international standard guidelines for ethics, conducting, monitoring and reporting of SRH research.
HRP publishes the report “Infertility Prevalence Estimates: 1990-2021”, the first report of its kind in over a decade.